Knee Meniscus Injuries
In this blog post our Cairns based physiotherapist Aaron Gandecha explains what the knee meniscus is and the latest evidence based management for degenerative tears.
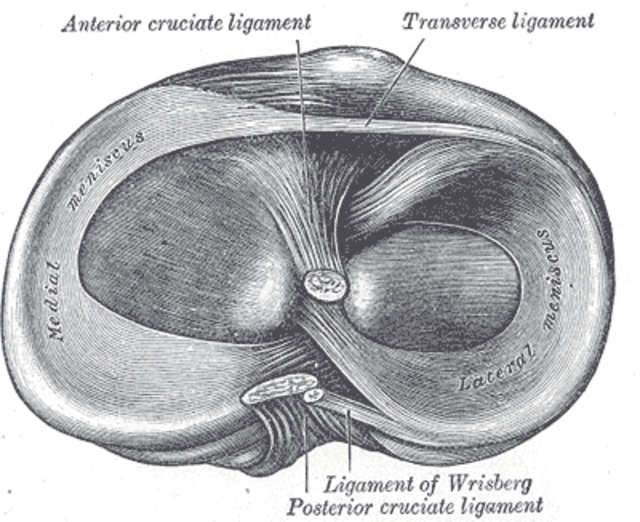
The knee meniscus is a series of two semi-circular structures which sit on top of the shin bone (tibia). It is an extremely important structure within the knee joint (the connection between the thigh and shin bones).
The meniscus has 3 main functions.
1) Increases conformity between the thigh and shin bone
2) Acts as a shock absorber to reduce the amount of load transferred through the bones
3) Provides stability to the knee by limiting extreme ranges of motion and aiding in joint proprioception
Tears of the meniscus are very common and are generally grouped into two categories, degenerative or traumatic.
Degenerative Tears
The meniscus has an extremely limited blood supply. Recent evidence from 2020, suggested that unlike other structures around the body such as bones, muscles and the intervertebral discs in the lower back, the knee meniscus has little to no potential for healing or remodelling as we reach adulthood.
For some individuals, this can mean a weakening of the meniscus over time. It is important to note that this is NOT solely down to "wear and tear”. Meniscal weakening is likely to occur due to a combination of factors such as genetics, age, sex, lifestyle, muscle strength, previous injury, body weight, other health conditions AND mechanical loading (“wear and tear”).
As the meniscus weakens it becomes susceptible to a tear. If a symptomatic tear does occur you may not be able to attribute it to a specific event, or you may notice the onset of pain from something completely innocuous such as walking or going to stand up.
As only part of the meniscus has a nerve supply, the tear itself may not actually be painful at all, in many cases it is the knee synovium (the glove that surrounds the knee joint) that becomes painful as it is irritated by the meniscal tear.
Many degenerative meniscal tears are completely asymptomatic. In one study of people over the age of 50 with no knee pain, 19% had a meniscal tear on MRI.
How are they Treated?
Well… it depends and the answer is complex, multi-factorial and unique to each individual!
All meniscal tears and all knees are not the same. More complex tears can cause not only pain, but instability, locking, catching, giving way, restricted range of motion and pain. However the exact same tear in somebody else, may be symptom free!
It therefore really does depend on the individual. If someone is getting persistent symptoms as mentioned above, surgery may be indicated.
Partial meniscectomy (removal of the torn portion of the meniscus) is one of the most commonly performed surgical procedures in the world!
However there is data showing that when comparing physiotherapy management with partial menisectomy, patient satisfaction, functional ability and pain outcomes at 2 years are around the same.
In addition there is increasing evidence that a partial meniscectomy may increase the risk of developing knee osteoarthritis. One study from 2021 found half of those who underwent the procedure developed knee OA within 5 years. This risk appears to be significantly greater in those that are obese.
It is therefore currently recommended that where possible, degenerative meniscal tears are managed conservatively with physiotherapy.
Meniscal Repairs
One other potential option is meniscal repair. The benefit of a repair is that the knee meniscus in retained rather than removed. It has been shown that repairs lead to better outcomes than removal and may half the risk of developing knee OA. However, it is still associated with greater overall risk of developing OA than no surgery.
A repair of the meniscus is commonly used in younger patients who have sustained a traumatic meniscal injury. Age was commonly considered the biggest roadblock as it was thought that those over the age of 40 would suffer from a significantly increased risk of surgical failure.
Whilst the evidence is limited, recent studies actually show no significant differences in failure rates dependent upon age.
Suitability for meniscal repair is more dependent on the type and location of tear (those located towards the outer edge of the mensicus tend to do far better), physical activity levels prior to onset of symptoms, the presence of other pathology within the knee and other health conditions.
Meniscal repairs are also likely to involve very strict postoperative instruction to protect the repaired tissue. It is not uncommon to be non weight-bearing after the surgery for at least 6 weeks.
Due to the time off of your feet they absolutely require extensive post operative rehabilitation.
Failure rates of meniscal repair are anywhere between 9 and 23% dependent upon the type of tear.
Physiotherapy Management
How we treat you with physiotherapy really depends on your symptoms!
When symptoms first occur it is not unusual to have a large amount of muscle guarding, muscle inhibition and even loss of range of motion. At this stage hands on physiotherapy treatments such as massage and joint mobilisation and guidance on suitable low level exercises may help.
As the knee becomes less irritable our focus becomes a lot more individualised!
The meniscus plays an important part in the function of the lower limb. Injury can lead to a whole host of muscle weaknesses, neurological changes, loss of proprioception (control), reductions in balance and changes in movement patterns. All of these factor can contribute to an increased amount of load passing through the joint, potentially causing further irritation and pain.
Our overall aim is restore your injured limb to the same function as the uninjured side.
Our aim in the management of degenerative meniscal injuries should be full recovery and return to your previous level of function!